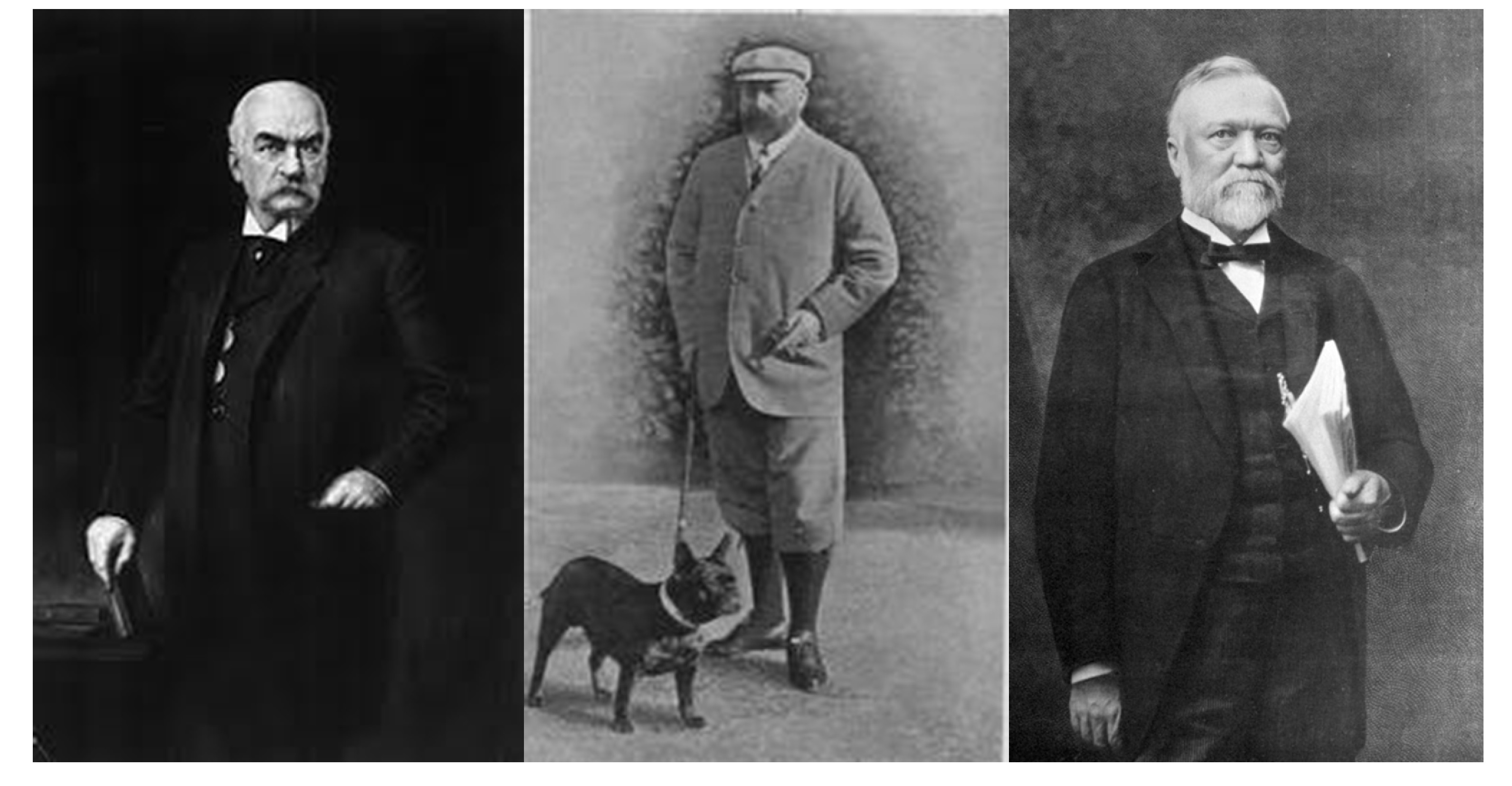
Our image of wellness and health has changed in the last two centuries. In the late 19th and early 20th century the healthy and wealthy looked like the men who appear in the picture below. By today’s standards we would consider these men fat or even obese.
- From left to right, J.P. Morgan, Edward VII and Andrew Carnegie represented what was considered a healthy figure at the end of the 19th century.
Back in their time these men were society’s elite, an example of success in life. Of the three only Edward VII died from the kinds of complications we associate with bad health decisions and obesity, indulging in 20 cigarettes and 12 cigars per day, gluttonous eating habits and dying from a succession of multiple heart attacks. The other two managed to survive their obesity.
Today we have a different human paradigm as seen in the image below. Obesity doesn’t fit with this picture. Yet today obesity is reaching epidemic proportions, and not just in North America, but worldwide.
Why? Because our obesity grows:
- As more of us move from rural to urban areas
- As we move from physical work to knowledge work
- As we add more labour-saving technology to our homes
- As we bring new entertainment technologies to our living rooms and dens
- As we rely more and more on drugs that have side-effects contributing to obesity
We eat saturated fats and sugar. We are less active physically than any previous generation. In 2012 according to a recent Australian study 1.5 billion of us are overweight. Of these 400 million are obese.
Our genetics contributes to this condition in part but our growing bulkiness stems from the combination of all of the issues described above. Since 1980 these behaviours and lifestyle changes have led to obesity growth rates of 300% in North America, parts of Europe, the Middle East, the Pacific Islands, Australasia and China. And there doesn’t appear to be an end in sight.
There are consequences. Obesity and being overweight comes with increased risk including (in alphabetical order):
- Cancer of the breast, colon, endometrium, kidney, gall bladder and prostate
- Cardiovascular disease
- Chronic musculoskeletal problems effecting joints such as knees and hips
- High blood pressure
- High blood cholesterol
- Hypertension
- Infertility
- Osteoarthritis
- Skin problems
- Stroke
- Type-2 Diabetes
Obesity in adults is accompanied by obesity in children. In a recent United Nations report it was estimated that 22 million children under five years of age worldwide were overweight.
Even more alarming is a correlation between obesity and Type-2 Diabetes and exposure to air pollutants. Recent studies reported by the American Diabetes Association indicate that exposure to particulate matter in the air leads to increased obesity and diabetes. The study concludes that exposure to particulate matter in the air results in inflammation in fatty (adiopose) tissue as well as insulin resistance and that this is contributing to the doubling of reported cases of diabetes over the last 15 years in the United States to almost 24 million.
There is a correlation between obesity and pharmaceuticals. So many medical conditions we treat with drugs that have an unwanted side affect — obesity. Drugs that treat depression, psychoses, and epilepsy are known to stimulate appetite. So do anti-viral and anti-HIV drugs. Steroids, progesterone and estrogen to treat autoimmune and hormonal imbalances also contribute to weight gain. We are, infact, medicating ourselves to obesity.
Effective Lifestyle and Eating Remedies for Obesity
It is in our nature to ignore a condition until it leads to more serious outcomes and that is the way most of us treat obesity and being overweight. As a result we treat the complications, medicating for all the diseases described above, rather than coming up with strategies to deal with the initial problem.
The easiest way to deal with obesity is through managing diet and changing lifestyle. To do this we need to:
- Change the type of foods we eat as well as the quantity. This involves increasing the amount low-fat and high-fibre foods we eat. It means more fruit and vegetables, more whole grains and nuts in our diet, less saturated animal-based fats, more unsaturated vegetable-oil fats, and less sugary foods. And it means eating less.
- Develop an active lifestyle involving daily exercise to burn the food we eat. This doesn’t mean becoming a marathoner. It does mean developing active hobbies, walking instead of driving, and cycling instead of using a car.
As a writer I am very aware of how my work environment can contribute to weight gain. I have watched my weight go up and down over the years. Today I am once more shedding pounds to reach my ideal weight, around 80 kilograms (176 pounds). I am about 7 kilograms away right now. How I’m doing it is by combining portion control in my eating with increased activity. I make a point of walking one hour every day to offset the long deskbound hours when I am doing research and writing. I conscientously take frequent breaks from my desk to walk from my office upstairs to our main floor or our basement. By doing this I hope to lessen the impact of sedentary work.
But even with diet and exercise overweight problems and obesity don’t necessarily go away. And if you are on a drug treatment program to deal with other maladies, you may find it very difficult to keep weight off.
In the University of Melbourne study in Australia that we talked about earlier in this blog, researchers tracked 50 overweight men and women with an average weight of 95 kilograms (209 pounds). The group was put on a 10-week low-calorie diet and on average lost 13 kilograms (29 pounds). At the end of the weight-loss period, body hormone levels changed leading to an average weight regain of almost 5 kilograms (11 pounds). So even when humans lose weight many regain a portion of it quickly. And it appears this has something to do with our body chemistry, the proteins that are part of us that determine when we are hungry and when we are not.
Can Science and Technology Save Us from being Overweight?
Two gastric endocrine hormones play a significant role in dealing with enhancing and suppressing our appetite. One is leptin. The other is ghrelin. Researchers study the interrelationship between these two in trying to understand why some people are more prone to obesity or eating disorders.
The hormones are truly a balancing act. Leptin regulates energy levels in the body by suppressing the desire to eat. It is an anorexigenic (as in anorexia) hormone. Ghrelin acts as a counterweight to leptin. If energy levels are low it encourages us to to eat. The term to describe the ghrelin hormone characteric is orexigenic.
Obese patients are orexigenic. They are leptin-resistant because they either do not produce enough leptin protein in their systems to stop them from wanting to eat or they produce too much ghrelin within their bodies which stimulates the appetite.
In studying the leptin-ghrelin cycle researchers at the Scripps Research Institute in La Jolla, California have identified a way to suppress grhelin using an antibody. Under the leadership of Dr. Eric Zorrilla, a neuroscientist who specializes in eating disorders, the Scripps research team has developed an antibody-based therapy that combine an anti-ghrelin with a carrier protein harvested from a mollusc, the Keyhole Limpet.

The protein, Keyhole Limpet Hemocyanin or KLH, is currently being studied as a carrier protein for cancer treatment vaccines to treat non-Hodgkins lymphoma, cutaneous melanoma, breast and bladder cancers. But what it can do for cancer also works when it is coupled with ghrelin antibodies. Currently being tested in animal studies, Scripps plans a human vaccine trial in the near future.
Is the future of obesity tied to a vaccine rather than dieting and lifestyle changes? For most of us who can control obesity and being overweight by changing diet and behaviour the obesity vaccine will probably never be something we need. But like so much of the progress we make in technology we may just choose the easy way out and get a shot to deal with being overweight.