April 15, 2014 – I’m a regular blood donor. My blood type is “A,” “Rh+.” That can tell you a lot about your origins. But that’s not what interests me. What I get excited about is the promise of finding a process by which we can end blood transfusions forever, mass producing all the blood we need rather than tapping the veins of donors every 56 days to keep an adequate blood supply in hospitals and clinics around the world.
There have been many attempts over the years to create synthetic blood, a product that mimics blood’s essential purpose as the transporter of of oxygen and other nutrients throughout the body. But in every case no equivalent to natural blood has emerged.
Making blood from stem cells, however, would be a game changer. The goal would be to create the equivalent blood type, group O, rhesus negative. This is a type of blood that we define as the universal donor, a product suitable for all transfusion recipients. You see my blood can only be given to those who are also A Rh+ or AB Rh+. There are a lot of people on this planet with A Rh+ blood so in donating I can help them. There are very few with AB Rh+ and even so I can help them as well. But if all of this sounds a bit confusing here is quick blood type primer.
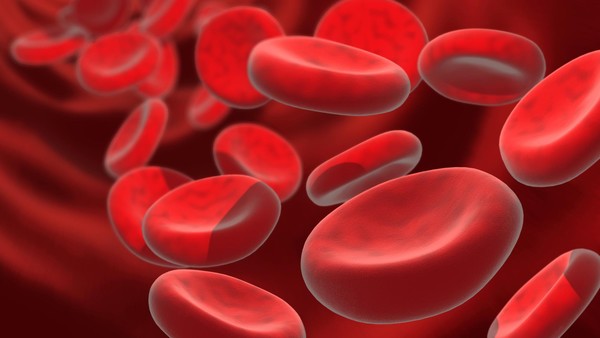
We have known since the early 20th century that not all blood is the same. That’s because the red blood cells each of us has contain different types of antigens. Antigens are sugars and proteins that can be found adhering to the surface of blood cells. Mismatched transfusions can trigger an immune system response. That’s why all who receive blood need to have their type identified before suitable donor blood can be dispensed. Our antigens are determined by our genetic makeup, our DNA. If our genes are not encoded for a particular sugar or protein then that antigen is absent from our blood cells. The absence or presence of these antigens determines the type of blood we have.
The identifying letters, “A,” “B,” and “O,” used here in North America and throughout much of the rest of the world (Russia and Eastern Europe use a numbering system) define the primary blood types. A secondary typing is known as “Rh.” And there are even more which we call subtypes, some of which are very rare. These are designated by the addition of a number beside the letter. So if you have your blood typed or if you choose to donate blood, you will be told that your blood is one of the following: A Rh+, A Rh-, B Rh+, B Rh-, AB Rh+, AB Rh-, O Rh+, O Rh-. Further testing may yield a sub-type such as A1, A1B, A2, A2B, and B1. These are among the 200 blood groups that modern science has identified.
Remember at the beginning of this posting I said that your blood type can tell you a bit about your origins. Here is a bit of blood geography lesson.
“A” blood type populations tend to be found in Central and Eastern European populations with one exception. The Blackfoot tribe in the United States happens to be predominantly type “A.”
“B” blood type populations are most commonly found in Asia, particularly China and India.
“AB” types are least common and found mostly in Japan, Korea and China.
“O” types, the most common are found in African, Hispanic and North American tribal populations.
The secondary blood typing “Rh,” which stands for rhesus factor, was first discovered in 1940 while testing inter-species blood transfusions between rhesus monkeys and rabbits., Rh+ is far more common than Rh-. Caucasian populations (European) tend to have the highest incidence of Rh- blood while Asian, Hispanic, Black, and North American aboriginal populations are predominantly Rh+.
Why is “O Rh-” considered the universal donor. Because both the “O” and the “Rh-” stand for the absence of the antigen proteins and sugars that cause immune responses.
Mismatching blood types has always had deadly consequences. Today such incidents are fairly rare. For example, in 2008 in the United States, 24 million transfusions were performed with 54 transfusion-related fatalities. In 2011 the number of transfusion deaths was 69. Before the turn of the 20th century mismatched blood deaths were common.
The goal of researchers in the United Kingdom, who have been working on producing blood from stem cells are trying to create a match to “O Rh-” for obvious reasons. This type of blood could be used by anyone. The researchers have chosen to work with embryonic and induced pluripotent stem cells (iPSCs). Starting with the embryonic type they can produce limited quantities of universal donor blood. But using iPSCs gives them access to much greater production volume. So the plan is to develop universal donor blood eventually from iPSCs. After four years the results are showing considerable promise with the first trials which they call “in-man,” scheduled for late 2016. “In-man” means exactly what it says. These trials will involve transfusing blood made from stem cells into human recipients.
One of the researchers in the program is Marc Turner, medical director of the Scottish National Blood Transfusion Service, describes the challenges and goal that lie ahead for the team. “Producing a cellular therapy which is of the scale, quality and safety required for human clinical trials is a very significant challenge, but if we can achieve success with this first in-man clinical study it will be an important step forward to enable populations all over the world to benefit from blood transfusions.”
In the meantime, I’ll still be donating blood every 56 days or so.