In the wars between those who advocate for vaccine and anti-vaxxers, the question of whether a person once infected gains lifetime immunity or not requires investigation. Our innate immune response to infection uses B-white blood cells (also called lymphocytes) to make the antibodies that search out and tag viruses and infected cells. Then the T and CD8-white blood cells find the tagged items and destroy them.
How Long Does Natural Immunity Last?
Our biological systems need a few days to engender an immune response as described above. And once an infection is defeated, that response remains vigilant for a period of time before beginning to fade. Just how long we are protected from being reinfected is still not a certainty.
A recent BBC article cites a Public Health England study that shows an active immune response remains with us for at least five months. In some cases, previously infected COVID-19 patients got reinfected within a year. A King’s College London study indicated a drop in antibody levels only three months after infection. But it also noted that B-cells retained a longer-term memory and could begin manufacturing antibodies if a second infection occurs.
As a side note of interest, the article mentions that B-cells for the Spanish Flu could still be detected in people 90 years after that early 20th-century pandemic. Also, the article described how T-cells against SARS, the coronavirus pandemic that struck in 2003, were still detectable in people 17 years after being infected. It further stated that T-cells that target the common cold (another coronavirus) could be helpful in fighting COVID-19.
Reinfections do occur. The likely explanation is the new infection is not from the same virus, but from a variant. An example of note, a recent Hong Kong patient had experienced reinfection four months after first contracting COVID-19. DNA analysis showed the second infection was a variant. That’s why the body’s immune system didn’t respond immediately.
Enter Vaccines, Adjuvants, and What They Do
Unlike our natural immune response, a vaccine is designed to give our body systems targeted instructions to fight one or more virus strains (vaccines that can handle two or more variants are referred to as multivalent).
The current COVID-19 vaccines, whether mRNA or adenovirus, are specifically looking for a spike protein found on the virus’s outer coat. That triggers what B-cells normally do, the production of antibodies which then tag all infected cells and viruses. A multivalent booster vaccine is less specific because it can look for a range of viral characteristics to target.
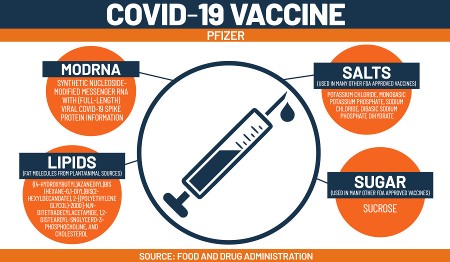
The current vaccines also contain ingredients designed to induce more potent immune responses. These are called adjuvants, which consist of ingredients developed in past vaccines that are known kickstarters for our immune system. Both the Pfizer and Moderna mRNA vaccines include nanoparticles that target the immune response. So do adenovirus vaccines like AstraZeneca and Johnson&Johnson.
What are the ingredients in adjuvants? They don’t roll trippingly off the tongue and include molecules of alum (a combination of aluminum and potassium) and toll-like receptor (TLR) agonists that go by such names as AS03 (an oil-in-water emulsion composed of squalene, polysorbate 80 and vitamin E), MF59 (a derivative of shark liver oil), and CpG 1018 (a modified phosphorothioate found in Hepatitis B vaccines).
The adjuvants act like an irritant to promote B, T, and CD8 cell production shortly after entering the body. I am convinced based on my personal level of “irritation” after getting my second dose of the Pfizer vaccine that the adjuvants knocked me for a loop for more than half a day. And now that I know what they are all about, I suspect that’s why my joints ached, I developed a headache, bone-weary tiredness, and hot flashes, all of it happening less than 24-hours after getting the shot. But the outcome was fine because the next day I felt great.
Vaccine studies show stronger immune cell responses than ones looking at natural infection responses. That’s why vaccines are so important in tackling a pandemic. That’s also why 320 different COVID-19 vaccines are under development or already being produced, distributed, and administered. With them, the chances are much better for those who are vaccinated to develop immune responses that last well beyond two years.
A final note, if the SARS 2003 coronavirus pandemic response is any indicator, when that virus vanished before a vaccine could be delivered, with or without one, our body’s T-cells should demonstrate long-term memories of COVID-19. With, however, our body’s memory will be that much stronger.