My blood type is A, Rh+. I know this because I was a regular blood donor for more than 35 years.
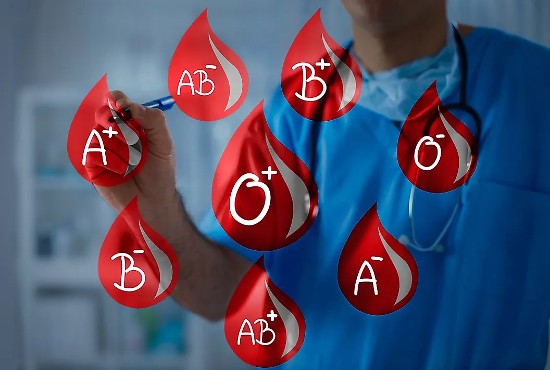
If you are unfamiliar with blood types, consider this a quick introduction before we look at the relationship between blood type and disease susceptibility.
What Defines a Blood Type?
Blood groupings used in North America and many other parts of the globe use a lettering system that differentiates types. They are A, B, AB, and O.
What is the difference among these types?
It is the presence of specific antigens (protein molecules attached to the blood cell surface) that define the groupings. Blood type A is red blood cells with an A antigen. Blood type B has B antigens. AB has both, and O has none. The presence of the RH protein is designated +. The lack of it is a -.
Blood plasma, the clear yellow liquid harvested by blood banks for transfusions also contains distinct antibodies (also proteins). Those with A blood have plasma containing anti-B. Those with B contain anti-A. AB has no plasma antibodies. O has both anti-A and anti-B.
And to make blood typing even more complicated over 600 and possibly more antigens are found in human blood with their presence or absence causing a potential mismatch for a blood transfusion recipient.
Did My Blood Type Make Me More Susceptible to COVID-19?
When SARS, the original coronavirus outbreak struck back in 2003, early research discovered that those with Type O blood appeared to be less susceptible to infection. Was it the lack of the A and B antigens making the difference?
Twenty years later researchers are finding a similar pattern in incidents of infection and blood type with people like me with Type A, being more susceptible. Why? Because Type A blood makes COVID-19 stickier in the presence of host cells.
COVID-19 in its most severe form is associated with blood clots. And it appears that Type A blood exhibits incredibly sticky characteristics in the presence of the virus. Why a respiratory virus causes this remains an unknown. Evidence shows, however, that the clotting factor, fibrinogen, is found in much higher levels than normal in COVID-infected patients with Type A blood.
Sticky red blood cells and increases in fibrinogen can lead to both small and large clots that can form in blood vessels. During COVID when we were being advised to stay at home, meant prolonged periods of inactivity. If you had COVID and worked at a desk during the lockdown your behaviour and blood type may have increased susceptibility to complications. Now when I look back at my behaviour during COVID I can see how long periods spent at this desk writing may have contributed to my worsening condition when I got COVID. The term is called “seat immobility syndrome” and I certainly imposed this condition on myself. the antidote is simple. Get up from your seat once an hour and move around which then gets the blood to circulate better reducing the risk of getting clots.
A study published in 2021, in Frontiers in Cellular and Infection Microbiology, looked at blood type susceptibility and mortality from COVID in a Delhi, India, hospital. It looked at 2,586 COVID-infected patients and concluded that those with A, B, and Rh+ were more susceptible than those with O, AB, and Rh-blood. There was no correlation in terms of severity or mortality.
Another 2021 article from Seminars in Vascular Surgery looked at a multinational dataset of COVID-infected patients and noted an emerging trend that those with Type A might be more susceptible to COVID infections but like the Delhi study, saw outcomes related to severity or mortality not impacted by blood type. It concluded that blood type screening, therefore, was not an effective triage tool for those ending up in hospital emergency rooms with COVID-19 symptoms.
COVID-19 Viruses May Find Blood Types A and B Sweeter
The receptor-binding domain (RBD) of the infamous COVID spike protein is possibly the area that makes the virus stick to cells states an article that appeared this August in the JAMA Network.
COVID’s RBD resembles galectins, carbohydrate-binding proteins, that are found in human and other animal blood. Some galectin proteins react to Type A, and B blood differently than with Type AB and O. And COVID’s RBD spike protein receptor appears to do the same, finding Type A and B blood to be more attractive, like flies to sticky honey. So should those of us with Type A and B blood be more worried about COVID infecting us?
Just under half of the world’s population have Type A and B blood which may mean greater susceptibility to COVID. But those with Type O and AB have also been getting infected by the virus. So, no matter what blood type you have, taking precautions is the route to go. Good sanitation, wearing a mask in indoor environments or in crowded venues outdoors where there are lots of people, and keeping up to date with the latest vaccines will minimize the risk.